Promoting the Applications of Dental MRI
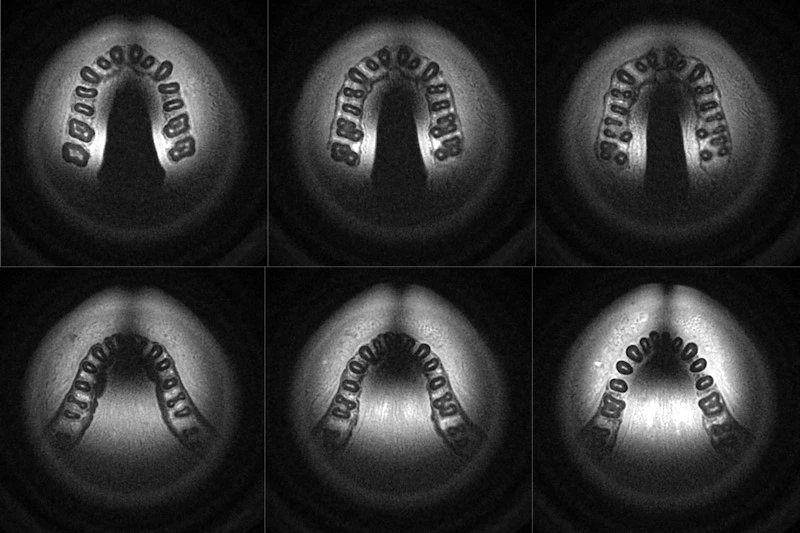
Palatal masticatory mucosa has been subject to extensive research work recently as it is the source for mucosal grafting. Its thickness varies among individuals, and preoperative assessment prior graft harvesting is mandatory. Recent research focuses on using dental MRI to accurately measure mucosal thickness and to locate the greater palatal artery to avoid its injury during surgery.

Soft tissue grafts are increasingly used for correction of bony defects in the alveolar ridge, for treating gingival recession and for creating soft-tissue support around implants. It could be difficult to harvest soft-tissue grafts with sufficient size while avoiding injury or interference with surrounding vital tissues. The anatomic variations are likely to increase the risk of such injury and subsequent complications.
The palatal mucosa contains the greater palatal artery, and its damage can result in haemorrhage, tissue necrosis or both. Bone sounding with periodontal probes (under local anesthesia) is commonly used to determine the mucosa thickness and the best location for graft harvesting. CBCT can also provide high-quality images to confirm the suitable area for taking a graft.
Dental MRI is growing more popularity as it eliminates radiation and can be used in a similar fashion to CBCT to create 3D images. Feasibility, accuracy and reliability in using MRI for assessment of palatal mucosa need to be tested.
A recent study has shown many advantages of dental MRI for assessment of palatal mucosa and locating greater palatal artery. Examination time was 15 minutes and intravenous contrast agent was not needed; thus the cost of the procedure was reduced and safety was enhanced. The use of of 3D images allowed for creating surgical guides by 3D printing.
The most effective area for harvesting soft tissue grafts are the molar regions followed by canine area. Zucchelli’s technique for connective-tissue graft recommends the minimal thickness of graft as 0.7 mm, which is still dependent on the individual variations between patients and recipient sites. There are many factors that govern the thickness, location and dimensions of the graft such as the anatomic variations and different branching patterns in addition to the distance from the cemento-enamel junction and the greater palatal artery. Neurovascular bundle need realistic view to determine the palatal mucosa thickness.
Dental MRI can be used for connective tissue graft assessment and implant planning on single image modality, while mapping the surrounding blood vessels. The us of MRI is still limited in patients with pacemakers or other metal implants in the body. The presence of metal fillings, dental implants and braces can hinder the use of MRI as imaging quality is impaired.