All-Digital Method for Condylar Repositioning
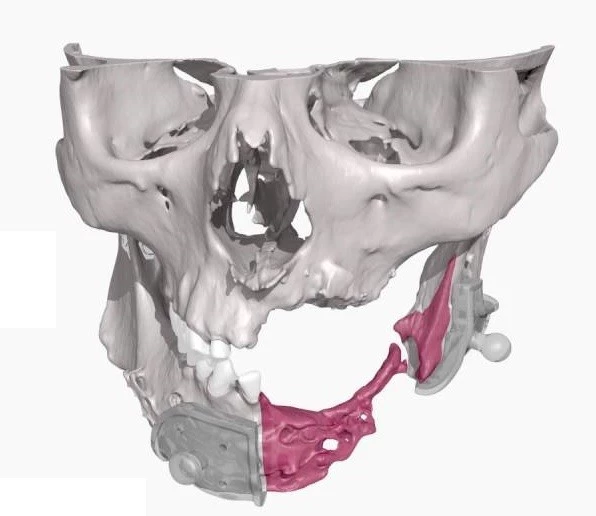
3D-printed models can be used for condyle repositioning to simulate reconstruction and orthognathic surgery in a simple and efficient way. This is one of several techniques for constructing fully-scaled 3D models of the skull and the jaws from CT scans and MRI. Such 3D-printed models are very helpful for preoperative simulation in case of maxillary/mandibular tumor or other deformities. The models can be fabricated for the mandible and maxilla individually or as single unit with fused jaws. When building a single model (with 1 temporomandibular joint), there is concern about poor operability on this model and possibility of bending the reconstructive plates. On the other hand, the 3D models created with separate mandible and maxilla possess better operability but still could be difficult to fully restore the position of the mandibular condyle after simulations.
Fully restoring the condylar position can be done with a device that maintains the configuration of the mandible through embedding magnets into the joint. Researchers in Japan test the reproducibility of an all-digital method for condylar repositioning through custom-made metal plates fabricated by CAD/CAM and computer simulations. This method is believed to replace the standard, commercially available reconstructive plates. The limitation of this method is the regulations and approval in addition to the need for robust training for the operators and technicians on constructing image-based anatomical structures.
The position of the mandible to the maxilla is anatomically governed by ligaments; so, when a proximal bone fragment with the ramus detaches, the dislocation force can cause postoperative jaw deformity or progressive condylar resorption. That is to say, any fault with the preoperative simulations would likely affect the postoperative outcomes.

This method is believed to work better with young operators who have greater interest in using 3D models and images. Such young operators are now used to working with 3D models for understanding anatomical variations and safety operations. Using such fully-scaled 3D models offer shorter and more accurate operation based on realistic preoperative simulation; it also facilitates better control on the extent of bone movement and explores ideal occlusion. In addition, 3D-printed models can allow for constructing temporary crowns and plates before surgery with high accuracy and reasonable cost.